
Healthy At Any Size? An Honest Discussion
Over 70% of adults are classified as overweight or obese. When you realize that just 40 years ago only 25% of the adult population fell into either of these categories, it’s fairly obvious we’re in the midst of an epidemic.
And yet, there are those who would say that obesity is nothing to be worried about. Not only is it nothing of concern, but it is something that should be championed.
Related - Is Fructose Making You Fat?
Sorry to burst the burgeoning bubble of grandeur around obesity, but the simple truth of the matter is that being overweight or obese causes a number of health problems.
Now, you might think that everyone, thin and thick alike, has some inherent risk for developing some kind of disease or chronic condition in their life.
And, you’d be right.
We all have a 100% risk of dying.
But, I’m not talking about dying from natural causes.
I’m talking about dying from things like:
- Heart disease
- Cardiovascular disease
- Cancer
- Chronic lower respiratory diseases
- Stroke (cerebrovascular diseases)
- Kidney disease
Diseases such as these are among the leading causes of death in humans, and they’re usually brought on (much sooner than they might occur, if ever) from a mixture of poor diet and severe physical inactivity.
Today, we’re going to look at the ways obesity significantly increases your risk of dying from some of these diseases and how much greater at risk you are for developing one of these diseases and dying from it.
Obesity, Chronic Disease, and Death
Heart Failure
According to the United States Centers for Disease Control and Prevention, roughly 6 million people are living with heart failure.
What is heart failure?
You might think it means that the heart stops working. It’s “tapped out” in a manner of speaking. But, that’s not quite what it means.
Heart failure is a chronic, progressive condition highlighted by an enlarged and/or weakened heart muscle and reduced blood-pumping efficiency. Essentially, the heart muscle cannot keep up with the demand for blood, oxygen, and nutrients.
As a result, individuals with heart failure can experience:
- Shortness of breath
- Weakness
- Fatigue
- Breathing complications when lying down
- Swelling in the feet and ankles
Researchers have found “evidence of a clear dose-response relationship between general and abdominal adiposity and heart failure incidence, and there was a 35% increase in the RR (relative risk) even in the overweight BMI range.” [2]
To be a bit more specific, researchers found there to be a 41% greater risk for developing heart failure for every 5-unit increase in BMI, and a 29% increase in relative risk per 10-cm increase in waist circumference. [2]
To top it off, they also found a 28% increase in the relative risk per 0.1-unit increase in waist-to-hip ratio. [2]
Anyway you spin it, if you are overweight or obese you have a substantially greater risk for heart failure.
These findings are backed up by a very recent 2019 study (including over 13,000 people) which observed that for every 5-unit increase in BMI, there was a ~30% greater risk of developing heart failure across all groups. [3]
This was after controlling for other comorbidities like high blood pressure, high cholesterol, and diabetes.
And, to make things just a tad grimmer, there is a 50% mortality rate for individuals with heart failure five years post-diagnosis.
So, what is it about obesity that increases the risk for heart failure?
Well, being overweight or obese is associated with a heightened risk of several other chronic conditions, including:
- hypertension, [4]
- insulin resistance, [5]
- diabetes mellitus, and [6]
- dyslipidemia [7]
Each of these increases the risk of heart attack and can, therefore, increase the risk of heart failure. [8]
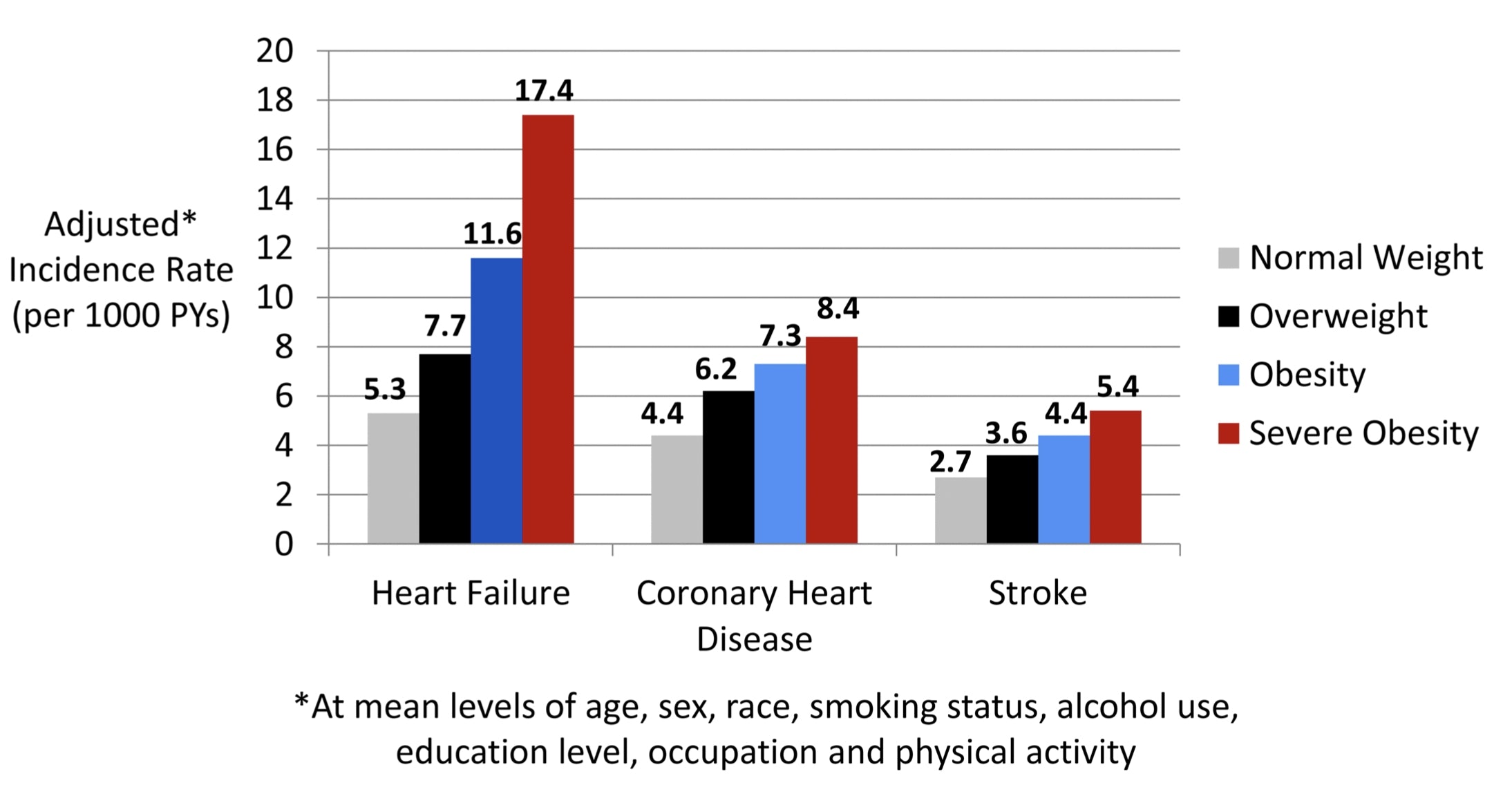
Figure 1. Association of BMI categories with adjusted incidence rates for different CVD subtypes. Incidence rates were calculated at mean levels of age, sex, race, smoking status, alcohol use, education level, occupation, and physical activity within the study population. BMI indicates body mass index; CVD, cardiovascular disease; PY, person‐year. [3]
Cardiovascular Disease
While you might think that heart failure and cardiovascular disease are more or less the same thing, they’re actually quite a bit different as cardiovascular disease typically refers to conditions that involve narrowing or blockage of blood vessels. This can lead to a heart attack, chest pain, or stroke.
Cardiovascular disease morbidity (having the disease) and mortality (dying from it) is greater in overweight and obese individuals, particularly those with greater abdominal adiposity (belly fat). [9]
Interestingly, abdominal obesity has been shown to be a risk factor for cardiovascular disease around the world.
Studies have found a strong association between BMI and stroke -- for every ONE-unit increase in BMI, there is a 4% increase in the risk of ischemic stroke, where the arteries to your brain become narrowed or blocked, causing severe blood flow reduction.
There’s also a 6% increase for hemorrhagic stroke, whereby blood vessels break and bleed into the brain. Within minutes, brain cells start dying. [10,11]
Researchers have also noted that 10 kg (22 lbs) higher body weight is associated with a 3.0 mm Hg higher systolic and 2.3 mm higher diastolic blood pressure. [12]
While these blood pressure increases might seem trivial, they actually lead to a 12% increase in risk of coronary heart disease and 24% increased risk for stroke. [12]
So, how does being overweight or obese contribute to the development and progression of cardiovascular disease?
Well, for starters, higher levels of body fat can contribute to high blood pressure, atherosclerosis (hardening of the arteries), atrial & ventricular enlargement, and inflammation (which increases fat buildup in the heart itself!).
In fact, visceral obesity may account for as much as 65%-75% of the risk for hypertension! [13]
Body fat also indirectly contributes to the development of cardiovascular disease, as it is linked to the development and progression of several disorders pegged as major cardiovascular disease risk factors, including:
- Sleep apnea,
- Dyslipidemia,
- Type 2 diabetes, and
- Metabolic syndrome
Researchers also suggest that the heightened occurrence of stroke in obese individuals may be due to the prothrombotic/proinflammatory state that frequently accompanies excessive body fat accumulation.
Cancer
Obesity increases your risk for several types of cancer, including: [14]
- Kidney
- Gallbladder
- Pancreatic
- Liver
- Prostate
- Breast
- Ovarian, and
- Stomach cancer.
To bring some granularity to how obesity increases the risk for these various cancers, let’s discuss some of the specific numbers as noted by researchers.
Kidney Cancer: Overweight or obese individuals are about twice as likely as normal-weight people to develop renal cell cancer, the most common form of kidney cancer. [15]
In fact, the increased risk of developing kidney cancer is independent of its association with high blood pressure in the obese.
Gallbladder Cancer: People who are overweight have ~20% increase in risk of gallbladder cancer, while the obese have a 60% increase in risk of gallbladder cancer compared to individuals of normal weight. [16,17]
Breast Cancer: Researchers have documented that for every 5-unit increase in BMI there is 12% increase in risk. [18] Among postmenopausal women, obese women have a 20%-40% increase in risk of developing breast cancer compared to their normal-weight counterparts.
Endometrial Cancer: Obese and overweight women are approximately 2-4x as likely as to develop endometrial cancer compared to normal weight women. Morbidly obese women are about seven times as likely to develop the condition. [19]
Liver Cancer: People who are overweight or obese are up to two times more likely to develop liver cancer than normal weight individuals. It’s also worth noting that the link between overweight & obese individuals and liver cancer is greater in men than women. [20,21]
How does obesity contribute to the development of cancer?
Researchers believe it centers around the systemic inflammation induced by large amounts of visceral fat.
Excessive amounts of body fat create a pro-inflammatory state in the body, which causes the pancreas to secrete too much insulin. At the same time, larger and greater amounts of fat cells lead to elevated estrogen production.
This trifecta of inflammation, elevated estrogen, and increased insulin production cause cells to divide (multiply) more frequently than usual. As a result of the rapid cell division, DNA damage can occur, which can turn into cancer.
Kidney Disease
Obesity has shown to be well associated with chronic kidney disease and abnormal renal function. [24] Studies have found that for every 5-unit increase in BMI, death caused by kidney disease increases by 60%. [22]
Other studies note that the rate of end-stage renal disease increased stepwise as BMI increased. [23] Researchers noted this link even after adjusting for confounding factors such as high blood pressure, diabetes, age, and smoking.
How does obesity impact the progression of kidney disease?
Well, obesity tends to coincide with elevated albumin excretion rates, which serve as a marker for early kidney function impairment and an increased risk of cardiovascular morbidity and mortality. [25]
This correlation occurs even in the absence of hypertension and diabetes, too.
Furthermore, obesity-related dyslipidemia can lead to progressive chronic kidney disease by encouraging inflammation and endothelial dysfunction. And, researchers have also observed an association between the decreased concentration of “good” HDL cholesterol in obese individuals and a higher incidence of chronic kidney disease.
Finally, research from Turkey found that high cholesterol and a higher BMI were associated with a lower glomerular filtration rate -- an indicator of kidney dysfunction. [25]
Respiratory Disease
Up until now, we’ve focused on the “heavy hitters” of disease states. The reason for this is that studies note that for every 5-unit increase in BMI (from 25-50) is associated with increased mortality from diabetes, stroke, chronic kidney disease, ischemic heart disease, and neoplasms. And, all-cause mortality was lowest when individuals have a BMI between 22.5–25 kg/m2. [27]
Above this range, mortality, on average, is about 30% higher for every 5-unit increase in BMI.
Well, there’s another “heavy hitter” to add to that list that may not seem as obvious -- respiratory disease.
On average, obese individuals have a 20% greater risk for dying from respiratory disease than individuals of normal weight. [30]
So, what exactly is respiratory disease?
In a nutshell, it’s a class of diseases characterized by impaired function of the lungs and other parts of the respiratory system. Examples of respiratory diseases include asthma, chronic obstructive pulmonary disorder (COPD), pneumonia, and lung cancer.
In fact, obesity is known to account for approximately 30%–50% of the variability in apnea/hypopnea index (AHI). The apnea/hypopnea is an index used to measure the severity of sleep apnea. [31]
Excessive body fat leads to worsening lung function and respiratory symptoms. It can also lower chest wall compliance and respiratory muscle endurance alongside increased airway resistance and the amount of work your body has to do to breathe. [28,29]
As a result, obese individuals can develop obstructive sleep apnea (OSA) and obesity-hypoventilation syndrome (OHS).
And, it’s also well known that difficulty breathing leads to poor sleep, and poor sleep has also been shown to contribute to weight gain by increasing levels of the hunger hormone (ghrelin) and decreasing concentrations of leptin (a satiety hormone). This begins a vicious cycle that only continues to feed itself over and over.
Furthermore, disordered breathing while sleeping has also been shown to be independently associated with insulin resistance and glucose intolerance, potentially leading to type 2 diabetes. [32]
Takeaway
Obesity is an epidemic marked by elevated risks of several chronic diseases. These increased risks stem from increases in the amount of fat tissue and the by-products generated from these larger and greater number of fat cells.
We will all die of something (preferably of natural causes), but your chances of living a longer, more enjoyable, and disease-free life get smaller and smaller, the larger and larger you get.
But, it doesn’t have to be that way. You are the master of your domain. You choose what you eat, when you eat, how much you eat, and how much you move.
Obesity is a death sentence, but it is one of the few things in life that we are all capable of avoiding or undoing.
References
1) Table 53 . Selected health conditions and risk factors , by age : United States , selected years 1988 – 1994 Total , crude Table 53 . Selected health conditions and risk factors , by age : United States , selected years 1988 – 1994 through 2015 – 2016 Trend Tables. (2017), 2016–2017.
2) Dagfinn, A., Abhijit, S., Teresa, N., Imre, J., Pål, R., Serena, T., & J., V. L. (2016). Body Mass Index, Abdominal Fatness, and Heart Failure Incidence and Mortality. Circulation, 133(7), 639–649. https://doi.org/10.1161/CIRCULATIONAHA.115.016801
3) E., N. C., Kunihiro, M., Mariana, L., Natalie, B., S., B. R., Gary, G., Josef, C. (2019). Obesity and Subtypes of Incident Cardiovascular Disease. Journal of the American Heart Association, 5(8), e003921. https://doi.org/10.1161/JAHA.116.003921
4) Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis.BMC Public Health. 2009; 9:88. doi: 10.1186/1471-2458-9-88.
5) Everson SA, Goldberg DE, Helmrich SP, Lakka TA, Lynch JW, Kaplan GA, Salonen JT. Weight gain and the risk of developing insulin resistance syndrome.Diabetes Care. 1998; 21:1637–1643.
6) Abdullah A, Peeters A, de Courten M, Stoelwinder J. The magnitude of association between overweight and obesity and the risk of diabetes: a meta-analysis of prospective cohort studies.Diabetes Res Clin Pract. 2010; 89:309–319. doi: 10.1016/j.diabres.2010.04.012.
7) Dudina A, Cooney MT, Bacquer DD, Backer GD, Ducimetière P, Jousilahti P, Keil U, Menotti A, Njølstad I, Oganov R, Sans S, Thomsen T, Tverdal A, Wedel H, Whincup P, Wilhelmsen L, Conroy R, Fitzgerald A, Graham I; SCORE Investigators. Relationships between body mass index, cardiovascular mortality, and risk factors: a report from the SCORE investigators.Eur J Cardiovasc Prev Rehabil. 2011; 18:731–742. doi: 10.1177/1741826711412039.
8) Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration. Cardiovascular disease, chronic kidney disease, and diabetes mortality burden of cardiometabolic risk factors from 1980 to 2010: a comparative risk assessment.Lancet Diabetes Endocrinol. 2014; 2:634–647.
9) Van Gaal LF, Mertens IL, De Block CE. Mechanisms linking obesity with cardiovascular disease. Nature. 2006 Dec;444:875–80
10) Lavie CJ, Milani RV, Ventura HO. Obesity and cardiovascular disease: risk factor, paradox and impact of weight loss. J Am Coll Cardiol. 2009 May;53(21):1925–32.
11) Din-Dzietham R, Liu Y, Bielo MV, et al. High blood pressure trends in children and adolescents in national Surveys, 1963 to 2002. Circulation. 2007 Sep;116(13):1488–96.
12) Akil L, Ahmad HA. Relationships between obesity and cardiovascular diseases in four southern states and Colorado. J Health Care Poor Underserved. 2011;22(4 Suppl):61–72. doi:10.1353/hpu.2011.0166
13) E., H. J., M., do C. J., A., da S. A., Zhen, W., & E., H. M. (2015). Obesity-Induced Hypertension. Circulation Research, 116(6), 991–1006. https://doi.org/10.1161/CIRCRESAHA.116.305697
14) "Obesity and Cancer." National Cancer Institute, www.cancer.gov/about-cancer/causes-prevention/risk/obesity/obesity-fact-sheet.
15) Wang F, Xu Y. Body mass index and risk of renal cell cancer: a dose-response meta-analysis of published cohort studies. International Journal of Cancer 2014; 135(7):1673-86.
16) World Cancer Research Fund International/American Institute for Cancer Research. Continuous Update Project Report: Diet, Nutrition, Physical Activity and Gallbladder Cancer. 2015.
17) Li L, Gan Y, Li W, Wu C, Lu Z. Overweight, obesity and the risk of gallbladder and extrahepatic bile duct cancers: A meta-analysis of observational studies. Obesity (Silver Spring) 2016; 24(8):1786-1802.
18) Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet 2008; 371(9612):569-578.
19) Setiawan VW, Yang HP, Pike MC, et al. Type I and II endometrial cancers: have they different risk factors? Journal of Clinical Oncology 2013; 31(20):2607-2618.
20) Chen Y, Wang X, Wang J, Yan Z, Luo J. Excess body weight and the risk of primary liver cancer: an updated meta-analysis of prospective studies. European Journal of Cancer 2012; 48(14):2137-2145.
21) Campbell PT, Newton CC, Freedman ND, et al. Body mass index, waist circumference, diabetes, and risk of liver cancer for U.S. adults. Cancer Research 2016; 76(20):6076-6083.
22) Prospective Studies C, Whitlock G, Lewington S, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet 2009;373:1083-96. 10.1016/S0140-6736(09)60318-4
23) Hsu CY, McCulloch CE, Iribarren C, Darbinian J, Go AS. Body mass index and risk for end-stage renal disease.Ann Intern Med. 2006; 144:21–28.
24) Praga, M., & Morales, E. (2017). The Fatty Kidney: Obesity and Renal Disease. Nephron, 136(4), 273–276. https://doi.org/10.1159/000447674
25) Soylemezoglu O, Duzova A, Yalcinkaya F, et al. Chronic renal disease in children aged 5-18 years: a population-based survey in Turkey, the CREDIT-C study. Nephrol Dial Transplant 2012;27 Suppl 3:iii146-51. 10.1093/ndt/gfs366
26) Liese AD, Hense HW, Doring A, et al. Microalbuminuria, central adiposity and hypertension in the non-diabetic urban population of the MONICA Augsburg survey 1994/95. J Hum Hypertens 2001;15:799-804. 10.1038/sj.jhh.1001266
27) Jad Saab and Steven P. Salvatore, “Evaluating the Cause of Death in Obese Individuals: A Ten-Year Medical Autopsy Study,” Journal of Obesity, vol. 2015, Article ID 695374, 7 pages, 2015. https://doi.org/10.1155/2015/695374.
28) Murugan, A. T., & Sharma, G. (2008). Obesity and respiratory diseases. Chronic Respiratory Disease, 5(4), 233–242. https://doi.org/10.1177/1479972308096978
29) Zammit C, Liddicoat H, Moonsie I, Makker H. Obesity and respiratory diseases. Int J Gen Med. 2010;3:335–343. Published 2010 Oct 20. doi:10.2147/IJGM.S11926
30) Collaboration, P. S. (n.d.). Body-mass index and cause-specifi c mortality in 900 000 adults : collaborative analyses of 57 prospective. The Lancet, 373(9669), 1083–1096. https://doi.org/10.1016/S0140-6736(09)60318-4
31) Crummy F, Piper AJ, Naughton MT. Obesity and the lung: 2. Obesity and sleep-disordered breathing. Thorax. 2008;63:738–746.
32) Franssen FME, O’Donnell DE, Goossens GH, et al. Obesity and the lung: 5 · Obesity and COPDThorax 2008;63:1110-1117.

Leave a comment